Glaucoma is a chronic eye condition that affects millions of people worldwide. It is characterized by increased intraocular pressure, which can lead to optic nerve damage and vision loss if left untreated. Despite advances in medical management, surgical intervention remains a vital aspect of glaucoma treatment. In this article, we will delve into the landscape of glaucoma surgery, exploring the past, present, and future of this ever-evolving field.
Understanding Glaucoma: A Brief Overview
Before delving into symptoms of glaucoma, it is crucial to have a basic understanding of the condition itself. Glaucoma encompasses a group of ocular disorders that share a common feature – progressive optic nerve damage. This damage is often correlated with elevated intraocular pressure, resulting from impaired fluid drainage. While the exact pathophysiology of glaucoma is complex and multifactorial, understanding its underlying mechanisms is essential in guiding effective surgical interventions.
The Pathophysiology of Glaucoma
Glaucoma primarily occurs due to an imbalance between the production and drainage of aqueous humor, the fluid that fills the anterior chamber of the eye. Various factors, such as age, genetics, and certain medical conditions, can contribute to this imbalance. Increased intraocular pressure puts significant stress on the optic nerve, leading to its gradual deterioration over time.
However, the pathophysiology of glaucoma goes beyond simple fluid dynamics. It involves a cascade of molecular and cellular events that further contribute to the progressive damage observed in glaucoma patients. Oxidative stress, a process characterized by an imbalance between the production of reactive oxygen species and the body’s ability to detoxify them, plays a significant role in glaucoma. The accumulation of reactive oxygen species can lead to cellular damage and impaired function, exacerbating the optic nerve damage.

In addition to oxidative stress, neuroinflammation also plays a crucial role in the pathophysiology of glaucoma. The activation of immune cells and the release of inflammatory mediators contribute to the degeneration of retinal ganglion cells, further compromising vision. Apoptosis, a programmed cell death process, is another key mechanism involved in glaucoma. The gradual loss of retinal ganglion cells through apoptosis contributes to the irreversible vision loss experienced by glaucoma patients.
See Also: The Latest Advancements in Glaucoma Surgery Techniques
The Impact of Glaucoma on Vision
Vision loss is the most concerning consequence of glaucoma. The condition typically progresses slowly, often without noticeable symptoms in the early stages. However, over time, glaucoma can lead to permanent vision impairment and even blindness if not effectively managed. The visual field defects associated with glaucoma can significantly impact a person’s quality of life, limiting their ability to perform daily activities and affecting their overall independence.
It is important to note that glaucoma does not solely affect central vision. Peripheral vision, which allows us to see objects outside the direct line of sight, is also compromised in glaucoma. This loss of peripheral vision can make it challenging to navigate through crowded spaces, drive safely, or even recognize familiar faces. The impact of glaucoma on vision extends beyond the physical limitations and can have emotional and psychological consequences as well.
Given the potential devastating consequences of glaucoma, early detection and treatment are crucial. While medical management remains the primary approach, surgical intervention plays a vital role, particularly in advanced cases or when medical treatments prove insufficient. Surgical procedures aim to reduce intraocular pressure, alleviate the stress on the optic nerve, and slow down the progression of the disease. By understanding the intricate pathophysiology of glaucoma, surgeons can tailor their interventions to address the underlying causes, offering patients the best possible outcomes.
The Evolution of Glaucoma Surgery
Glaucoma surgery has come a long way since its inception. Early techniques focused on creating a new outflow pathway to reduce intraocular pressure. These invasive procedures, such as trabeculectomy and tube shunt surgeries, aimed to improve aqueous humor drainage and alleviate pressure on the optic nerve.
Early Techniques in Glaucoma Surgery
Trabeculectomy, introduced in the 1960s, quickly became the gold standard procedure for controlling intraocular pressure in glaucoma patients. This surgical technique involves creating a new drainage channel by excising a portion of the trabecular meshwork, allowing aqueous humor to bypass the conventional outflow pathway. Trabeculectomy, although effective, is associated with various complications, including hypotony and bleb-related issues.
While trabeculectomy was a significant advancement in glaucoma surgery, alternative early techniques also emerged in an attempt to reduce intraocular pressure by modifying aqueous humor dynamics. Peripheral iridectomy, for example, involved surgically removing a portion of the iris to improve aqueous humor flow. Similarly, cyclodestruction aimed to decrease intraocular pressure by destroying the ciliary body’s ability to produce aqueous humor. While these procedures demonstrated some success, they often lacked long-term efficacy and carried significant risks.
Modern Advances in Surgical Treatment
Advances in surgical techniques and technology have revolutionized glaucoma surgery. Minimally invasive glaucoma surgeries (MIGS) now offer a safer and more predictable alternative to traditional procedures. These innovative approaches provide a middle ground between more invasive surgeries and purely medical management, offering improved outcomes and a faster recovery time.
In MIGS procedures, tiny incisions are made to implant microstents or devices that facilitate aqueous humor drainage. These surgeries are typically performed in conjunction with cataract extraction, reducing the need for additional invasive procedures and enhancing patient convenience. The use of microstents, such as the iStent, allows for the creation of a controlled and predictable outflow pathway, effectively reducing intraocular pressure. MIGS procedures have gained increasing popularity in recent years due to their lower complication rates, shorter surgical times, and faster visual recovery.
Furthermore, advancements in imaging technology have greatly improved surgical planning and precision. High-resolution imaging modalities, such as optical coherence tomography (OCT), allow surgeons to visualize the structures within the eye with remarkable detail. This enables them to accurately identify the areas that require intervention and tailor the surgical approach accordingly. The integration of OCT into glaucoma surgery has revolutionized the field, enhancing surgical outcomes and reducing the risk of complications.
Overall, the evolution of glaucoma surgery has been driven by a constant pursuit of safer and more effective treatment options. From the early techniques of trabeculectomy and peripheral iridectomy to the modern advancements in MIGS and imaging technology, glaucoma surgeons continue to refine their approaches to provide optimal care for patients. As research and innovation continue to push the boundaries of what is possible, the future of glaucoma surgery holds even more promise in improving patient outcomes and preserving vision.
Current Surgical Options for Glaucoma
When it comes to glaucoma surgery, different approaches cater to varying patient needs and disease severity. Trabeculectomy remains the gold standard for more advanced cases, offering excellent intraocular pressure control. However, the associated risks and postoperative care requirements make it less suitable for all patients.
Trabeculectomy: The Gold Standard
A trabeculectomy involves creating a new drainage pathway by creating a small hole in the sclera, beneath the conjunctiva. This surgery allows aqueous humor to bypass the trabecular meshwork and form a filtering bleb. While trabeculectomy can effectively lower intraocular pressure, it carries the risk of complications, such as hypotony, bleb-related issues, and surgical site infection.
Minimally Invasive Glaucoma Surgeries (MIGS)
MIGS procedures have emerged as a valuable addition to the glaucoma surgical armamentarium. These procedures are often performed concurrently with cataract surgery, making them an attractive option for patients with both conditions. MIGS devices, such as the iStent and Hydrus Microstent, offer a less invasive approach for enhancing aqueous humor outflow while minimizing complications.
While MIGS procedures have shown positive outcomes, they may not be suitable for all patients. Factors such as disease severity, anatomical considerations, and previous surgeries must be taken into account when determining the most appropriate surgical approach.

The Future of Glaucoma Surgery
The landscape of glaucoma surgery continues to evolve, with promising advancements on the horizon. Emerging surgical techniques aim to address current limitations and offer improved outcomes for patients.
Emerging Surgical Techniques
New surgical techniques, such as canaloplasty and endocyclophotocoagulation, hold promise in enhancing aqueous humor drainage by targeting different pathways. Canaloplasty involves the dilation and tensioning of Schlemm’s canal, improving its functionality and facilitating outflow. Endocyclophotocoagulation offers a minimally invasive approach to reduce aqueous humor production by selectively damaging ciliary processes.
Other experimental techniques, such as gene therapy and stem cell transplantation, are being explored for their potential to repair damaged optic nerves and restore visual function. While still in the early stages of development, these cutting-edge approaches offer hope for the future of glaucoma treatment.
The Role of Technology in Glaucoma Surgery
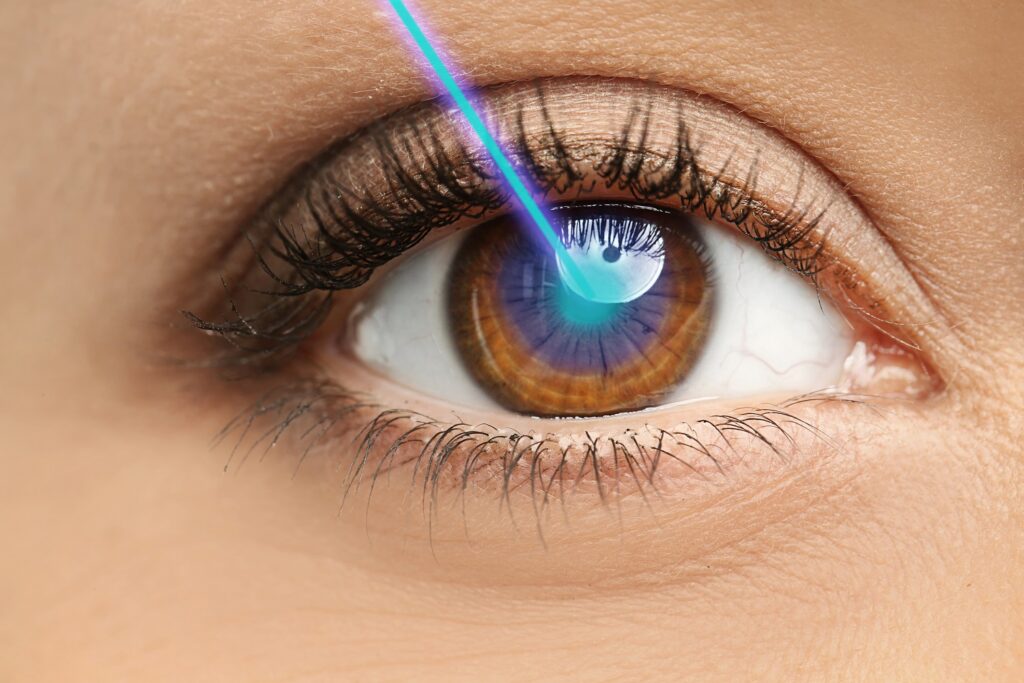
Technological advancements are playing a vital role in enhancing the precision and safety of glaucoma surgeries. Laser-assisted techniques, such as selective laser trabeculoplasty (SLT) and micropulse laser trabeculoplasty (MLT), offer an alternative to traditional surgeries by using laser energy to target the trabecular meshwork and improve aqueous humor outflow.
Additionally, intraocular pressure monitoring devices and imaging technologies, such as optical coherence tomography (OCT) and ultrasound biomicroscopy (UBM), provide valuable information for guiding surgical decision-making and assessing postoperative outcomes. The integration of artificial intelligence and machine learning algorithms holds further promise for optimizing surgical planning and improving long-term patient outcomes.Patient Considerations in Glaucoma Surgery
Choosing to undergo glaucoma surgery is a significant decision that requires careful consideration of various factors. It is essential for both patients and healthcare professionals to evaluate the potential risks and benefits of surgical intervention.
Evaluating Surgical Risks and Benefits
Glaucoma surgeries, like any surgical procedure, carry inherent risks. These risks may include infection, bleeding, hypotony, cataract formation, and visual disturbances. Patient-specific factors, such as age, overall health, and disease severity, must be taken into account when weighing the potential benefits against the surgical risks.
Open and honest communication between the patient and their ophthalmologist is crucial to ensure the patient’s understanding of the risks and realistic expectations post-surgery. Careful consideration of individual circumstances allows for personalized treatment plans that optimize patient outcomes.
Post-Surgery Care and Expectations
Postoperative care plays a vital role in the success of glaucoma surgery. Patients must adhere to a prescribed regimen of eye drops, oral medications, or both to prevent complications and optimize outcomes. Regular follow-up visits allow healthcare professionals to monitor the patient’s intraocular pressure, assess healing, and address any concerns.
It is essential for patients to have realistic expectations regarding the outcomes of glaucoma surgery. While surgery can effectively lower intraocular pressure and slow disease progression, it does not guarantee complete vision restoration and may not eliminate the need for ongoing medication or surveillance.
Eyes on the Future: A Bright Outlook
The landscape of glaucoma surgery is continually evolving, driven by advancements in surgical techniques, technology, and our understanding of the disease itself. As research and innovation continue to progress, the future of glaucoma surgery holds promise for improved outcomes and enhanced quality of life for patients.
Understanding the pathophysiology of glaucoma, the impact of the condition on vision, and the available surgical options is essential for both patients and healthcare professionals to make informed decisions regarding treatment. By staying informed and embracing emerging technologies, we can continue to aim for better outcomes and a brighter future in the fight against glaucoma.

